What the data actually say about COVID-19 and neurodegeneration
No, SARS-CoV-2 is not a prion disease... but it can damage your nervous system.
A few days ago, a Twitter thread went viral after sharing a link to a recent review paper on a potential connection between SARS-CoV-2 infection and prion disease. The tweet was framed as a press release, claiming that infectious disease experts believe COVID may cause a “rapidly degenerative, always fatal brain disease”. In order to prevent the spread of misinformation I will not link to the thread here, but as of 1 PM EST on May 24th, the tweet had garnered over 10.3k likes and 1.7M views. Many people, especially those who are medically vulnerable, are understandably alarmed by such a frightening assertion considering most people have been infected by COVID. I, too, found this thread alarming – because it lacks a fundamental understanding of major concepts in biology and biomedical science, and by misrepresenting a hypothesis paper as a major medical discovery intended to provoke panic, this type of thread threatens to delegitimize the high-quality research being published about COVID-19 and the nervous system.
This is also an excellent opportunity to break down how I like to fact check these types of assertions. So here we are – debunking this misinformation one step at a time.
Prions – what does amyloid have to do with it?
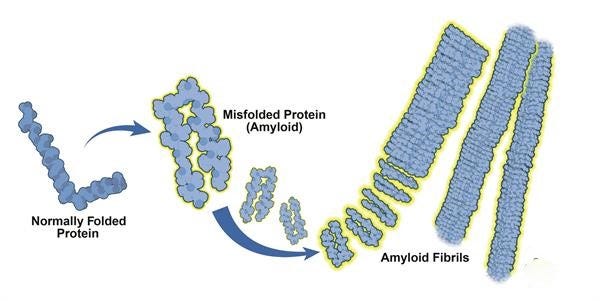
Let’s start off by reviewing what exactly a prion disease is and the biological processes involved, shall we? In simple terms, a prion is a type of amyloid protein – a signaling or structural molecule that becomes misfolded in a way that makes them stick together, forming clumps of self-propagating malfunctioning proteins. Prion diseases are very rare but severe conditions in which a particular misfolded protein can “seed” amyloid prion formation and induce neurodegeneration, which ultimately results in death. The idea that an individual protein can act as an infectious agent is still a novel discovery – even the smallest viral genomes encode a handful of proteins, which they require in order to reproduce.
Prion diseases have been observed in several mammalian species including cows, sheep, and deer. All of these conditions involve an abnormally folded version of the major prion protein (PrP), which is found in its normal configuration throughout the body floating around in the cell membrane. In humans, there are a few very rare genetic disorders with mutations of the PrP gene that make them more susceptible to amyloid formation, including conditions like fatal familial insomnia. This state of PrP-aggregate neuronal damage in humans is called Creutzfeldt-Jakob disease (CJD). Bovine spongiform encephalitis (BSE), sometimes called “mad cow disease”, represents a unique type of prion disease transmission – namely that people appear to develop BSE years or sometimes decades after consuming meat products contaminated with brain matter. Because misfolded PrP is a protein and not a virus or bacteria, it’s not susceptible to degradation by standard disinfection and sterilization procedures like ethanol and heat. There is also evidence toward amyloid conformations of other proteins playing a role in other neurodegenerative conditions like Alzheimer’s disease, although this remains a widely debated topic.
Now, let’s start breaking down the tweets a little bit:
1. Framing intended to misrepresent content in order to manufacture panic
Right off the bat, this is being framed is a news story when it is actually a Twitter thread by a layperson and not based around an actual publication with data to support their claims. This quote is unattributed and does not appear to exist, as both Google and PubMed searches for “COVID prion disease” only returns a handful of articles discussing the impact of COVID-19 on CJD, including the hypothesis paper in the next tweet which broadly discuss the way inflammation induced by COVID can precipitate neurodegenerative disorders, similarly to how COVID appears to induce diabetes in certain patients. While there is plenty of evidence showing that COVID-19 infection can result in acute and long-term neuroinflammation in some individuals, to my knowledge there is no direct evidence suggesting a major neurodegenerative phenotype in post-acute COVID syndrome. Instead, I found a handful of case studies that documented 6 patients total who developed CJD post-COVID infection, with various proposed hypothesis centered around neuroinflammation.
2. Immediately makes incorrect claims about prion diseases
As discussed earlier, CJD refers to the neurodegenerative disorder observed in human patients as a result of spontaneous or inherited mutations in PrP protein. “Mad cow disease” refers to Bovine Spongiform Encephalitis (BSE), a clinically distinct syndrome and one of the first highlighted points on the CDC’s informational page about prion diseases.

3. Frames hypothesis paper as scientific evidence
As you can see in the tweet above, the paper linked here is a hypothesis paper called “SARS-CoV-2, long COVID, prion disease and neurodegeneration”. Clicking through, you’ll see that A) this was first published in September 2022, B) does not contain any data, C) does not make any claims about COVID causing a de novo prion disease, and D) focuses on the role of inflammation in neurodegenerative disorders.
4. Does not link to the original data source on S1 spike containing prion-like regions, proceeds to misinterpret said original paper
I believe the original poster here is referring to a 2022 paper published in Nature Communications titled “Neurotoxic amyloidogenic peptides in the proteome of SARS-CoV2: potential implications for neurological symptoms in COVID-19”. In this paper, the authors used bioinformatic approaches to scan the genome of SARS-CoV-2 for any regions that might be able to form amyloid-like structures, and identified two short fragments from ORF6 and ORF10, proteins called “open reading frames” as they have no obvious roles in viral replication. Note that this is NOT spike protein – although S1 has been shown to induce amyloid fibrin clotting in the blood, this is a fully distinct phenomenon from any kind of prion disease that I discussed at length in a previous blog post. They then assembled these proteins in vitro and used them to treat cultured neuroblastoma cells, which resulted in reduced cell number relative to untreated cells. This is concerning, definitely – but a hypothetical peptide being toxic to cells grown in culture is a far cry from showing that COVID-19 infection in humans induces a neurodegenerative process via prion formation. Although the review paper cites a handful of case studies detailing patients who developed CJD following a COVID infection, they are all individual reports without any mechanistic or causational insight. Additionally, I found a single paper from 2021 that performed similar modeling experiments to show that spike protein may be able to form complexes capable of interacting with amyloid precursor protein, a molecule involved in Alzheimer’s disease progression... when using computational models. To date, we still do not have a very complete understanding of how the SARS-CoV-2 virus may interact with the nervous system.
The thread goes on to discuss the links between COVID-19 infection and new-onset neurodegenerative disorders – this IS true, although again the links provided here are for news articles and not for primary scientific data. Considering researchers have long hypothesized that some cases of conditions like Alzheimer’s disease may involve a viral trigger, this is not necessarily surprising information. It doesn’t seem clear whether COVID-19 infection triggers an existing predisposition to this kind of condition, or if it can act as the predisposition itself. More research in this area is desperately needed, despite the recent termination of the public health emergency in the US.
The thread ends with this tweet, the sentiment of which I wholeheartedly agree with:
I believe the original poster behind this thread has the right intentions, wanting to draw attention to the public health crisis that continues escalating by the day. In many countries including the United States, our government has embraced an approach to public health that celebrates thousands of unnecessary deaths per week as “back to normal”. Millions of medically vulnerable people across the world have been forced into a life of isolation, watching the people around us write off our lives and livelihoods as the cost of the new normal. Every chain of transmission prevented matters, and it has never been more important to look out for your neighbors and friends by using some basic preventative measures when you’re out in public spaces, like respirators and air filtration devices.
However, making unfounded inflammatory claims about a virus that we already know can drive long-term problems delegitimizes this cause. A majority of those seeing and reacting to tweets like this are either people who work directly with post-viral illness patients, people who are ill themselves, or people with other lived experience of the illness. Circulating false information insinuating that an already sick and very vulnerable group of people may also develop a fatal brain disease not only reduces the credibility of other legitimate medical discoveries, but also adversely impacts the very people it is trying to help by literally telling them they are going to die without any evidence. The situation is already dire and there is no reason to drum up panic about hypothetical and unsubstantiated claims. When encountering claims like this, it’s never a bad idea to pause before hitting the “retweet” button and evaluate whether or not the information is coming from a credible source.
For any readers interested in learning more about the interaction between SARS-CoV-2 and the nervous system, here are a few papers to start with:
Nervous system consequences of COVID-19. Spudich and Nath (2022), Science
The neurobiology of long COVID. Monje and Iwasaki (2022), Neuron
Long COVID: major findings, mechanisms and recommendations. Davis, McCorkell, Vogel, and Topol (2023), Nature Reviews Microbiology


New subscribers here. Contracted Covid in March 2020. Still have lingering aftereffects in October 2023. Devastating disease. Some aftereffects are neurological and some cardiological,. They are the most serious. The others, like fatigue and shortness of breath are just irritations that I've gotten used to. Being an infovore ex- academic, I collected as many articles as I could find and download on Covid from early 2020 on-most from the preprints. Hundreds of articles, but I never noticed any that linked Covid and BSE or prions. Thanks for the analysis. I notice this newsletter seems dormant. I hope you reactivate it! You were performing a valuable service and one needed now more than ever
I have an alternate view on lung physiology that dismisses the notion of oxygen and carbon dioxide gaseous exchange
The article is titled
We breathe air not oxygen
I take you though all the steps that lead to this statement
Including how oxygen is manufactured
How oxygen is calibrated
Eg medical oxygen has 67parts per million of water contamination
Why oxygen is toxic, dehydrates and damages the alveoli
Lung physiology requires the air at the alveoli to reach 100% humidity
Can you see the problem?
The new take on lung physiology:
The lungs rehydrate the passing RBCs with iso tonic saline solution as they pass through the alveoli capillary beds
RBCs change from dark contracted dehydrated to plump bright hydrated form as they soak up the iso tonic saline solution the bursting alveoli bubbles throw upon the capillary sac
The airway mucosa conditions the breathe with salt and moisture
Find the article
Jane333.Substack.com